OrbisRx – Simplified solutions delivering better Medicaid outcomes
We’re OrbisRx®, and we combine fresh approaches and innovative strategies, backed up by the decades of experience of Navitus Health Solutions. Thanks to our multifunctional modules and secure API, we bring modern digital speed and ease to a system that often feels behind the times.

State Medicaid Agencies (SMAs) are at a crossroads
As Medicaid evolves and budgets tighten, SMAs are under increasing pressure to do more with less — striving to deliver high-quality care while navigating shrinking budgets and rising complexity. But the outdated technology these systems run on is no longer just an inconvenience — it’s a barrier to effective care.
It’s time for SMAs to move away from this outdated structure to an integrated solution, letting them deliver clinical outcomes that are both optimal and in budget.
Our cutting-edge tools to modernize Medicaid management
OrbisRx Analytics
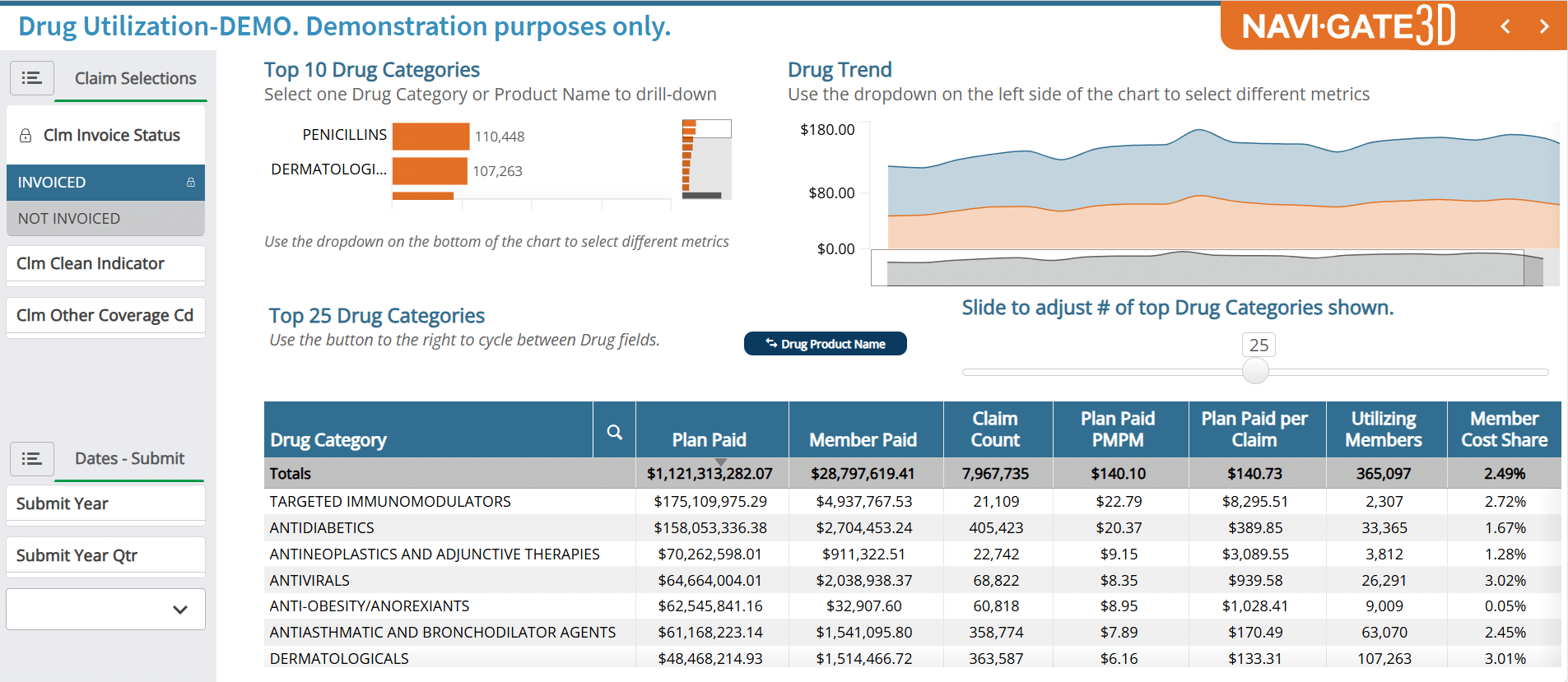
The OrbisRx Analytics Module empowers SMAs with clarity into their data and actionable insights – critical tools to effectively manage pharmacy spend, produce smarter, data-driven decisions and deliver pharmacy benefits to their most vulnerable populations.
The Analytics module offers:
This access to real-time information gives an SMA the most accurate data and the ability to deliver better results.
Our Analytics in Action
OrbisRx Claims
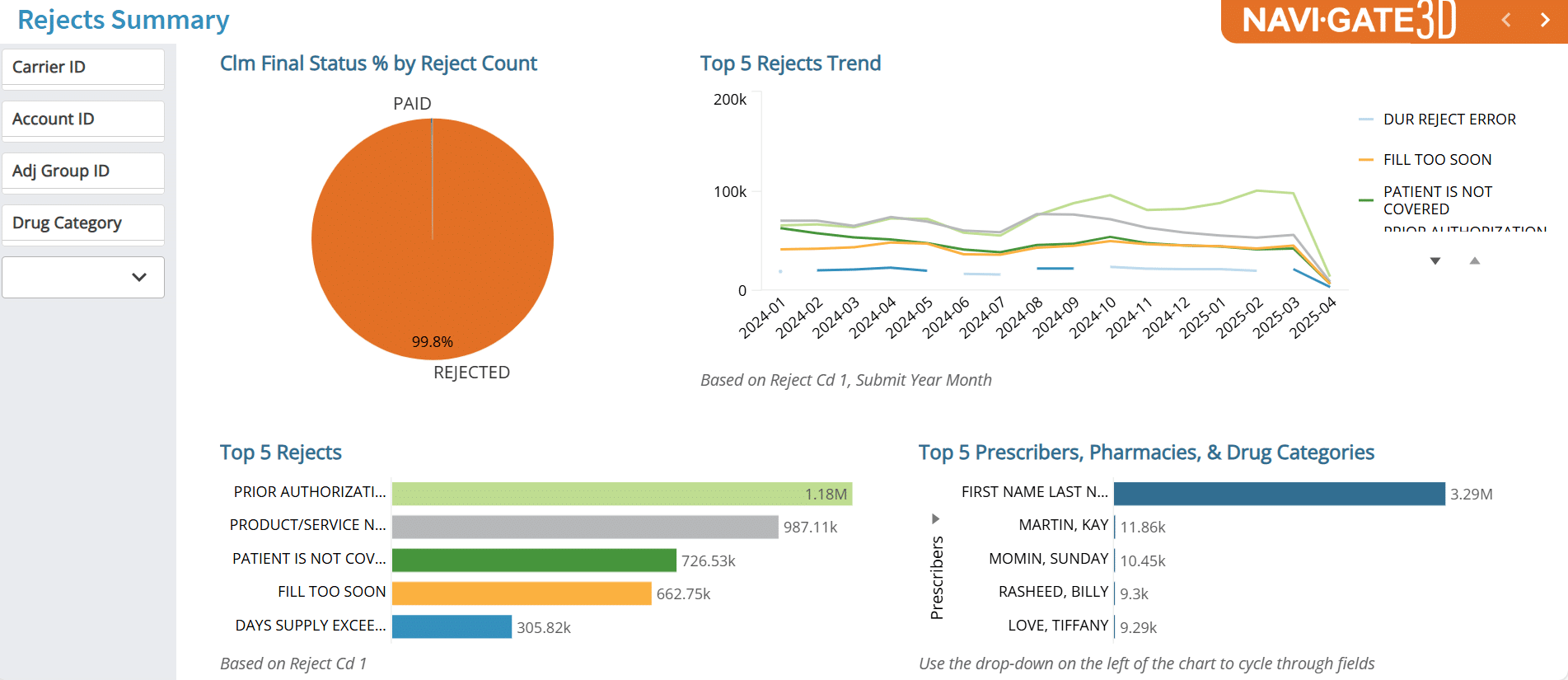
The OrbisRx Claims Module provides a dynamic, 360⁰ view of pharmacy data. Through a secure, web-based GUI, the tools within the Claims module make it faster and easier to monitor data, including:
SMAs have access to a full view of Medicaid claims processing information from Navitus, so they can build custom reports that meet their needs, including utilization by pharmacy, provider, member, drug class and more. This enables SMAs to have greater visibility into real-time trends impacting their pharmacy claims.
OrbisRx Prescriber Portal
The OrbisRx Prescriber Services Module is a cutting-edge, digital solution designed to streamline and modernize Medicaid prescribing workflows. Built on secure, API-driven technology, this module connects seamlessly with trusted systems like LexisNexis and integrates directly with the Navitus prior authorization (PA) platforms.
Prescribers gain instant access to real-time member data, coverage validation tools and electronic prior authorization capabilities — all in one intuitive interface. By replacing outdated paper-, fax- and phone-based processes with streamlined digital data, our prescriber portal empowers providers to make faster, more informed decisions. This ensures Medicaid members receive the right medications without delay.
This digital data includes:
OrbisRx Rebates
States need to drive toward the lowest-cost medications for Medicaid beneficiaries and resolve balance issues quickly.
The OrbisRx Rebates Module provides a state-of-the-art, API-supported platform, enabling states to:
Our cloud-based technology platform includes:
By providing clarity into Medicaid drug claims, this module enables states to make timely, informed formulary decisions and get outstanding claims resolved fast.